The term “gynecomastia” is derived from the Greek and translates as “woman-like breasts”. An enlargement of the male breast is more common than generally assumed, affecting between 40–60 % of the male population. It can affect one or both breasts. Already in puberty, the male breast often enlarges due to hormonal changes and may cause great discomfort to the young adults. Fortunately, pubescent gynecomastia often resolves itself spontaneously. Certain drugs (e.g. anabolic steroids, drugs containing oestrogen, alcohol, marijuana (cannabis, hashish) and certain diseases (e.g. cancer, liver dysfunction) can cause gynecomastia. In the majority of cases, however, the cause of gynecomastia is still unknown (idiopathic gynecomastia). In these cases, surgery is the only solution.
Considerations
When to consider gynecomastia:
- The surgical correction of gynecomastia is indicated when otherwise treatable causes for enlarged breasts are ruled out and if one or more of the following conditions are met:
- You suffer from the size and shape of your breasts.
- One breast is noticeably larger than the other.
- Your wellbeing and self-esteem is adversely affected by gynecomastia.
- The size of your breasts limits your physical and sporting activities.
- You are otherwise healthy and emotionally stable.
Consultation
A prerequisite to a successful operation is careful planning. This starts with a personal consultation at the AARE KLINIK.
- Communication of wishes and expectations ascertain what you would like to improve.
- Explanation of the possibilities and scope of the operation.
Examination:
- Medical history is taken.
- Physical examination is performed.
- Digital photos are taken.
- Desired breast size and shape are discussed as well as the position and size of the nipples.
- Pre-existing asymmetry in the breasts or chest, skin quality and existing scars are examined.
- Individual factors and personal wishes help in jointly deciding the choice of appropriate surgical technique, the position of incisions and resulting scars.
- Based on this, an individual treatment plan is drawn up and goals of the operation are discussed and defined.
- Risks and possible complications are discussed and documented.
To plan the operation and to make a risk assessment we require:
- Full medical history (pre-existing conditions and previous surgery).
- Current diseases (high blood pressure, diabetes, thyroid dysfunction, etc.).
- Allergies or aversion to medications.
- Any important medical reports.
- Please bring any important medical information (in particular anything relating to your breasts, e.g. mammography) along to the consultation and inform the surgeon if you have a history of breast cancer in your family.
- If you are planning to lose a significant amount of weight, this should be considered when planning a breast gynecomastia.
- It may be advisable to wait for the stabilisation of your weight before surgery is undertaken.
- Depending on your age, personal and familial risk factors, it may be advisable to have a mammography (X-ray examination of the breast) or sonography (ultrasound examination of the breast) before undergoing a surgical treatment of gynecomastia.
Procedure
If the breast consists mainly of fat rather than glandular tissue, then gynecomastia can be treated by liposuction. The ultrasound-assisted liposuction (UAL) is particularly effective for the removal of the dense fatty tissue of the male breast. The actual breast tissue cannot be suctioned, but has to be surgically removed. This is normally achieved through a short incision at the border of the areola. For very large breasts, or where there is a lack of skin elasticity, excess skin may also need to be removed. In most cases, it is possible to remove excess breast skin around the areola (periareolar tightening) with inconspicuous scars. At the AARE KLINIK we prefer to use a minimally invasive ultrasound-assisted liposuction (UAL) with the VASER® system to remove the fatty breast tissue. If necessary, remaining glandular breast tissue and/or the excess skin is then removed surgically. In this way, the length of surgical scars can be minimised.
Breast reduction in gynecomastia is performed under general anaesthesia as an outpatient procedure or over-night stay at the AARE KLINIK or as part of a short hospital stay. The surgery usually takes around 2 hours. If, in addition to liposuction, glandular tissue or excess skin needs to be removed, then drains are frequently inserted to evacuate blood and wound secretion from the wounds after the operation. These are removed after a few days.
Risks
When the procedure is performed with proper indications and surgical techniques, severe complications, such as infection, healing problems or circulation disorders of the breast tissue (e.g. loss of the nipple) are rare. However, in individual cases, a longer treatment or another operation may be required. Every patient should be informed of all the benefits, risks and possible complications involved.
The lighter complications that usually heal without consequences include bruising (hematoma), wound fluid accumulation (seroma) and swelling. Severe bruising may necessitate surgical removal. Numbness of the breast skin and nipples are common side effects, but usually only temporary if they do occur.
General risks
- Haematoma (bruising), bleeding and swelling
- Seroma (accumulation of wound fluid)
- Healing problems or infection
- Wound breakdown/dehiscence (separation of wound edges)
- Injury of nerves or vessels
- Numbness in area of operation (temporary or permanent)
- Circulatory problem of breast skin or nipple (skin slough)
- Scars
- Slight asymmetry
- Unsatisfactory aesthetic result
- Secondary surgery
- Thrombosis or embolism
Overall male breast reduction is a safe procedure when undertaken by an experienced plastic surgeon and patients are mostly satisfied with the results. You can help to minimise the risks by following the advice of your surgeon.
Preparation
Our aim is to make the time before and after your surgery as comfortable as possible. By following a few tips you can support our care:
- To aid the healing process, avoid smoking for two weeks before and after the operation.
- Avoid medication that increases the risk of bleeding, like aspirin, non-steroidal anti-inflammatory drugs, as well as vitamins and homeopathic remedies for two weeks prior to the operation.
- Breast reduction is mostly performed as an outpatient procedure under general anaesthesia.
- Make sure that you can be collected and cared for by someone for 24 hours after the procedure.
- In some cases it may be recommended to stay overnight as an inpatient in hospital.
Day of surgery
In most cases, gynecomastia surgery is performed under general anaesthesia as an outpatient procedure or with an over-night stay at the AARE KLINIK. In individual cases, when necessary, the procedure can be undertaken in an affiliated private hospital.
- During surgery you will receive various medications for your wellbeing.
- Usually breast reduction in gynecomastia is performed under general anaesthesia.
- For your safety, your heart rate, blood pressure, oxygen supply etc. are monitored during the operation.
- At the end of surgery, drains are usually inserted to prevent the accumulation of blood and serous fluid in the wound.
- After surgery, the wound is dressed and a special compression bandage or compression vest is applied
- You will be taken to the recovery room, where you will have continued monitoring until you awaken and are able to get up.
- You will be allowed to return home after a few hours.
- If you are an inpatient, you will remain in the recovery ward under surveillance until the following day.
- Already on the day of the surgery you should get up regularly for a few minutes in order to minimise the risk of thrombosis.
- The level of pain after breast reduction is not severe and can be compared with muscular pain.
- You are advised to take mild pain relief that reduces swelling and should be continued for several days after surgery.
- In case of an ambulatory procedure, you should have someone to care for you continuously for 24 hours postoperative.
- We also provide the option of an over-night inpatient stay at the AARE KLINIK in a single room with a personal nurse care, if needed.
After surgery
- It is important to realise that recovery from an operation varies for every individual.
- In the first days after a breast reduction, you should rest. Do not raise your arms above shoulder height, and do not lift heavy objects.
- As a rule, you need to sleep on your back for a few days.
- Only take the prescribed painkillers and avoid any medication that contains aspirin or other blood-thinning substances.
- Wear the special compression vest continuously for a total period of 4–6 weeks as per our recommendations.
- Physically demanding and sporting activities should be avoided for several weeks.
- In the first 2–5 days after the procedure, a feeling of tension and light pain will be felt in the region of the surgery.
- Breast skin and nipples may feel numb or hypersensitive in the beginning. This is usually temporary.
- However, it may take weeks or months, in some cases even longer until sensation returns to normal.
- Slight swelling and bruising in the area of ??breast usually subsides within 2–3 weeks.
- Typically you will be back on your feet a couple of days after surgery and be able to resume your daily activities.
- Drains are removed in the first days after the operation, after which you can take showers again.
- Full baths and excessive heat (e.g. sauna), however should be avoided for several weeks until swelling has receded.
- Most stitches will dissolve by themselves and do not need to be removed.
- Non-dissolvable stitches are removed after one week.
- You will probably be able to start work again one week after surgery depending on the kind of breast reduction and the kind of activities required in your job.
- After removal of the sutures, we recommend the start of an intensive skin and scar care with rehydrating creams and light massage.
- In individual cases it may be useful to have special treatment with silicone gel or silicone pads over a period of 2–3 months.
- The fresh scars should be protected from UV radiation for at least six months, in order to prevent increased pigmentation.
- After surgery you will be examined at the AARE KLINIK at regular intervals, so that the healing process can be assessed until the final result is achieved.
Outcome
- Your breasts may be swollen for some time after surgery. It may take several weeks until the bruising and swelling disappears.
- Scars might be a bit red for several months or appear pigmented, but this will fade with time until the scars and are barely visible.
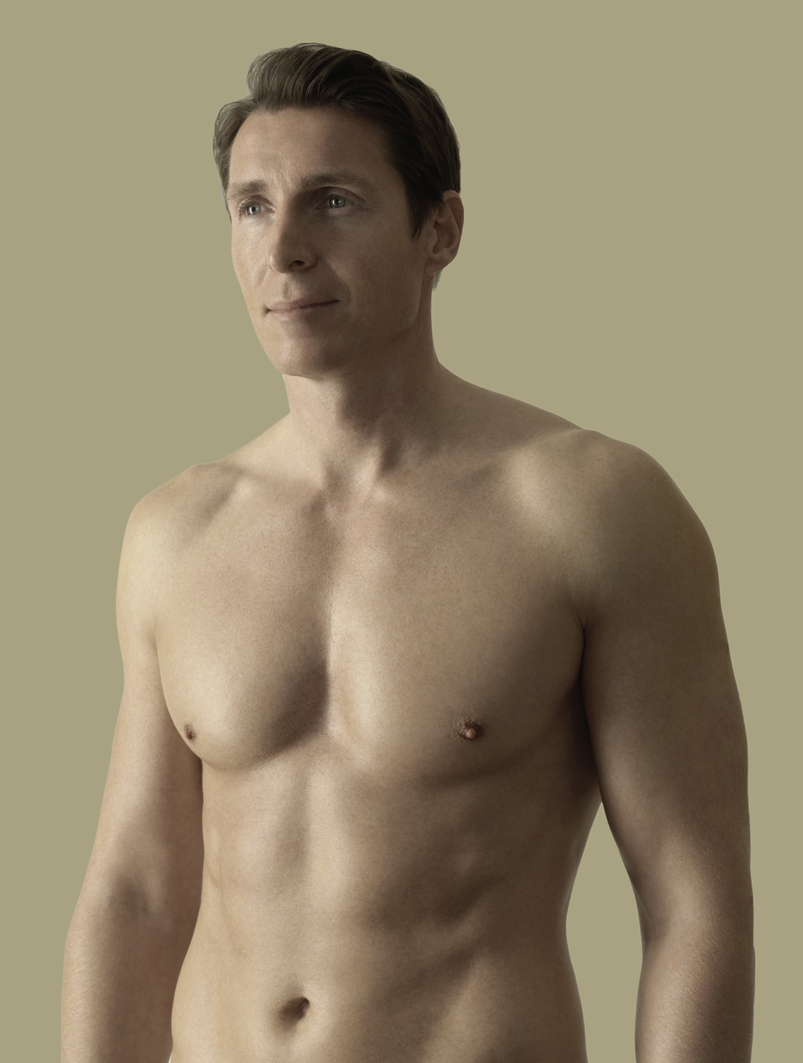
- The result of a breast reduction in gynecomastia is a flatter, firmer chest with improved chest contour and visibility of chest muscles that creates a more masculine body image and often improves self-confidence.
- The effect of the surgery is usually long lasting. However, a significant increase in weight after surgery can create a gynecomastia-like effect (pseudo-gynecomastia).
Costs
In cases of a true gynecomastia (enlargement of breast glands), breast correction is mostly medically indicated. In this case, the treatment costs are usually supported by health insurance, if a prior cost estimation is given.
However, when the condition is due an excess of weight (pseudo-gynecomastia), then the surgery is considered as cosmetic and the costs have to be carried by the patient.
The decision for, or against reimbursement depends on the recommendation of the medical officer in each individual case.
The cost of an aesthetically motivated breast reduction is variable and mainly depends on the complexity of the operation and the facility in which the surgery is performed (hospital or AARE KLINIK). A more accurate cost estimate can therefore be made only after a personal consultation.
The costs are composed of:
- Surgical fee (including consultation and post-operative care)
- Anaesthesia fee
- Technical infrastructure costs (AARE KLINIK/hospital)
- Inpatient hospital costs
- Compression vest
- Medication
- Diagnostics (laboratory, ECG, scans, etc.)